About Ventricular Tachycardia
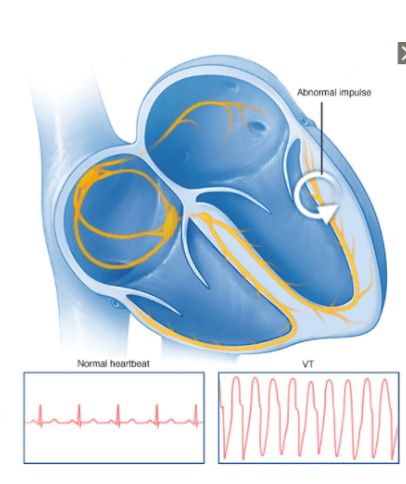
Ventricular Tachycardia (VT) is a rapid heart rhythm that occurs when the electrical stimulus originates within the Ventricle instead of the Sino-Atrio Node (SA Node) found in the atrium.
The stimulus for VT is often a particular area within the ventricle, causing a “re-entrant circuit” where the stimulus overrides the normal electrical stimulus. This consistent stimulus may lead patients to have a rapid but regular heart rate. However, this rapid heart rate may not allow sufficient time for the ventricles to fill with blood, leading to a reduction in cardiac output, low blood pressure and other symptoms such as dizziness, vertigo or syncope, and an altered level of consciousness.
Episodes of VT may last short periods of time but can last many hours at a time. Occasionally these episodes may start quickly and end spontaneously. This rapid heart rate is considered a medical emergency and would require emergency care.1
Causes of Ventricular Tachycardia (VT)
The most common cause of VT is structural changes to the ventricle, this may be caused by damage to the heart muscle after a myocardial infarction / ischemic event or cardiomyopathy (enlarged heart) of any cause.
Under normal circumstances, the stimulus for a heartbeat originates within the Sino-Atrial Node (SA node) in the atrium. Abnormal (damaged) myocardial tissue may lead to a scar formation within the heart wall that can facilitate a “reentrant electrical pathway” where an electrical stimulus continues to excite the ventricle in a cyclic fashion and produce a rapid heart rate that is regular. Other conditions that may increase the risk of VT are:
- Hypertrophic Cardiomyopathy (HOCM),
- Dilated Cardiomyopathy (any cause),
- Post ventricular surgery scars / incisions,
- Arrhythmogenic Right Ventricular Dysplasia (ARVD),
- Chagas disease, and
- Congenital conditions.2
Other non-structural causes of VT may be:
- Inherited Genetic Channelopathies such as Long QT syndrome,
- Electrolyte abnormalities (such as low potassium),
- Systemic diseases that can affect the heart muscle (myocardium),
- Sarcoidosis
- Amyloidosis
- Systemic Lupus Erythematosus
- Drug toxicity such as Digoxin (used for irregular heart rates),
- Cocaine and methamphetamine abuse,
- Use of some drugs that increase QT interval of an ECG.3
Signs and Symptoms of Ventricular Tachycardia
Patients with VT may present with a variety of symptoms ranging from mild palpitations to no cardiac output requiring Cardiopulmonary Compressions (CPR). In general, most patients will present awake with the following symptoms:
- Palpitations,
- Syncope / dizziness,
- Shortness of breath,
- Hypotension (low blood pressure),
- Chest pain and tightness, or
- Unconsciousness.
Diagnosis of Ventricular Tachycardia
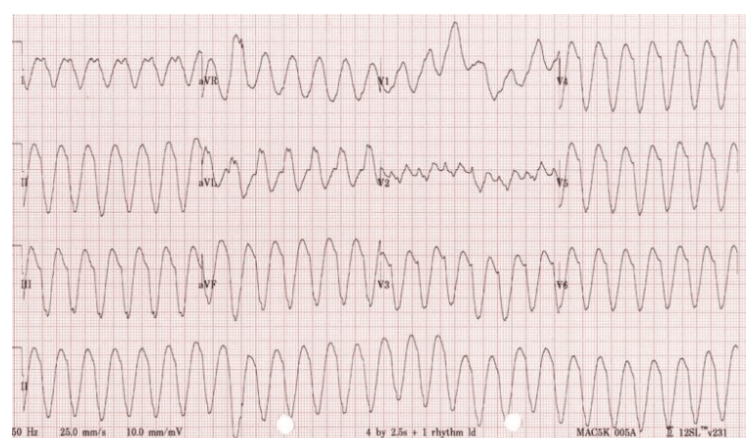
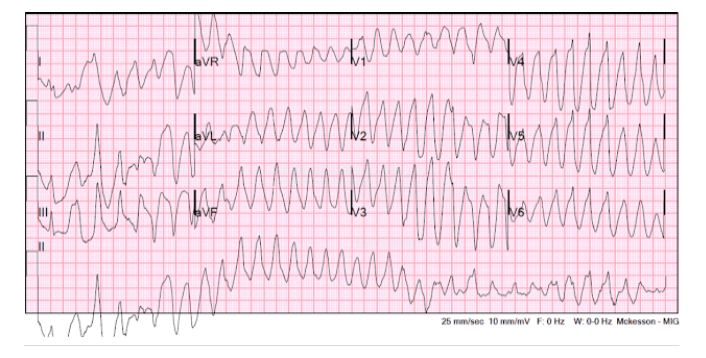
VT is diagnosed on a 12 lead Electrocardiograph (ECG). It will show a broad complex rhythm that is more likely to be regular with a rate of > 100 bpm. The diagnosis and symptoms correlation will usually confirm the presence of the condition. VT may be divided into the following forms of VT, each with its own classification (please note that there are other forms of VT than those discussed below).
An echocardiogram (Echo) may also be used to identify the presence of structural abnormalities that may cause VT, and also review the pump effectiveness of the heart, often referred to as the ejection fraction (EF). Patients with an EF < 35% may be considered at high risk of sudden cardiac death.
Monomorphic Ventricular Tachycardia
Generally, originates from a single focus within the ventricle, and is therefore regular, with a consistent heart rate, often > 100 bpm.
Polymorphic Ventricular Tachycardia (PVT)
Differs from monomorphic VT as there may be multiple areas of stimulation (or foci) that cause the rapid heart rate. The irregular nature of the heart rate is due to multiple areas of the stimulation from within the ventricle. The rhythm may be considered unstable due to the irregularity of the heart rate. Polymorphic VT may also include a different form of VT known as Torsades de Pointes (turning of the point). This form of PVT may also have other abnormalities such as long QT interval.5
Treatment for Ventricular Tachycardia (VT)
VT can be self-limiting and many patients might not be aware of the condition as the symptoms may be short-lived and not present on electrocardiograph (ECG) upon arrival for assessment. Treatment may be dependent on the cause of the VT. For the purpose of this site, treatment for VT will be divided into stable VT and unstable VT.
Immediate treatment for patients with VT will depend on the level of urgency and is therefore categorised into stable or unstable VT. Diagnosis of VT is usually made from an electrocardiograph demonstrating a broad complex tachycardia. This clinical urgency is often determined by the following:
- Heart rate,
- Blood pressure, and
- Level of consciousness (awake or unconscious).
Unstable VT
For those patients with very poor cardiac output, low blood pressure, and an altered level of consciousness, basic life support should be administered immediately and urgent help sought (ie. an Ambulance service).
In an unstable patient with an altered level of consciousness and poor cardiac output treatment will include:
- Cardiopulmonary resuscitation (if no palpable pulse),
- Electrical Cardioversion to restore normal electrical conduction via resetting the Sino-atrial node.
Once the event has been terminated, a medication (or multiple medications) that reduces the irritability of the ventricle or stabilises electrical activity may be used. This will depend on the clinical circumstances of each patient.
Stable VT
Many patients with VT will be awake and aware of the symptoms as outlined previously. In this case, first-line treatment may likely be to initiate an anti-arrhythmic medication, once this medication has been administered, the heart rate should return to normal, acceptable limits.7
Ongoing Management of Ventricular Tachycardia (VT)
VT can be a common arrhythmia in patients with heart failure and/or structural heart diseases, as well as, those with genetic conditions such as Long QT syndrome or HOCM. This condition will typically be managed by a cardiology team which may include (but is not limited to) a:
- Cardiologist,
- Heart Failure Specialist,
- Electrophysiologist, and
- General Practitioner.
The treatment may be divided into two categories:
Medical management
This may include medication that aims to control the heart rate and prevent VT from occurring. This type of medication prescribed can depend on the cause of the VT. A patients’ Cardiology team will work closely with their General Practitioner to review this ongoing program at home with a regular Specialist review when required.
Procedural management
This may include a number of potential procedures in order to prevent the recurrence of VT, in the case that a pathway/circuit is the likely cause of this condition:
- Insertion of Implanted Cardioverter Defibrillator (ICD). This is a device implanted in a patients chest that has the ability to sense, detect and treat VT when it occurs. These devices may also be able to deliver a rapid “overdrive pacing” therapy that can often end the VT by breaking the cycle that’s causing the VT, ultimately restoring a more acceptable heart rate. Should this not be successful, the ICD may deliver a “shock” to the heart to reset the electrical activity, similar to what may occur in a procedure called Electrical Cardioversion.There are two commonly available ICD’s, one with a lead that sits within the heart which is called a transvenous ICD system (TV ICD), and the alternative, which uses a different approach where the defibrillation lead sits external to the heart, usually within the chest wall above the ribs/sternum, and is called a Subcutaneous Implantable Cardioverter Defibrillator (SICD).
Transvenous ICD
*All content on Hope For Hearts does not endorse or promote any brands or devices and is only intended for educational purposes. Patients should always consult individual health matters with a medical professional.
Subcutaneous ICD (S-ICD)
*All content on Hope For Hearts does not endorse or promote any brands or devices and is only intended for educational purposes. Patients should always consult individual health matters with a medical professional.
Australian and New Zealand Guidelines for CRT
Another form of procedural management of Ventricular Tachycardia is,
- Ventricular Tachycardia (VT) Ablation. This is a procedure where a small electrical catheter is placed into the heart via the groin veins and the electrical activity of the heart may be mapped to identify where the abnormal circuit that is causing VT might be. Once this is identified the abnormal tissue/circuit may be destroyed using radiofrequency ablation to isolate the area, resulting in this area no longer able to stimulate the abnormal rhythm.8
Understanding Cardiac Ablation
*All content on Hope For Hearts does not endorse or promote any brands or devices and is only intended for educational purposes. Patients should always consult individual health matters with a medical professional.
