Implantable Cardiac Device for Heart Failure Management
Device Management
Many patients with HF also have ventricular dyssynchrony, which may not facilitate coordinated ventricular contractions and reduce cardiac output. This dyssynchrony can further impair cardiac function and may present on surface ECG as prolonged QRS duration. Patients with a Left Bundle Branch Block and QRS duration of > 120ms may benefit from Cardiac Resynchronisation Therapy or CRT. There has been compelling clinical evidence from randomised controlled trials that demonstrates that CRT can improve symptoms and cardiac function, reduce hospitalisations and mortality1.
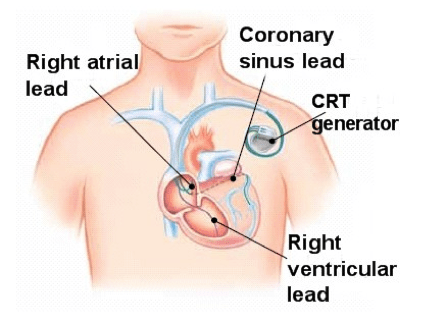
In typical CRT, there are three leads connected to a pacemaker or defibrillator, that aim to resynchronise the atria and the ventricular contractions. One lead sits in the right atrium, one the right ventricle, one in the coronary sinus over the left ventricle. The aim is to stimulate the right and left ventricles together and improve cardiac function.
Australian and New Zealand Guidelines for CRT
Patients may be considered for CRT if the following criteria are met:
- Patients with HFrEF and sinus rhythm, LVEF < 35% and QRS duration > 150ms
- Optimal medical therapy ongoing and EF has not improved despite this optimal treatment (usually after a minimum of three – six months)
- They are considered likely to live beyond the next 12 months
CRT Pacemakers will only sense and pace the heart as required. CRT Defibrillators have an inbuilt capacity to deliver CRT but also detect and treat life-threatening arrhythmias such as ventricular tachycardia or ventricular fibrillation. The devices can deliver different types of therapy depending on the rhythm detected3.
Patients with heart failure are at a high risk of sudden cardiac death (SCD) and this is thought to be associated with malignant ventricular tachycardias’. The implantation of a CRT device with the ability to deliver Anti-Tachycardia Pacing (ATP) or defibrillation has been demonstrated to reduce mortality4.
Clinical trials to support CRT/Device Therapy for SCD
CARHF: https://www.nejm.org/doi/full/10.1056/nejmoa050496
Companion: https://www.nejm.org/doi/full/10.1056/NEJMoa032423
SCDHeFT: https://www.nejm.org/doi/full/10.1056/nejmoa043399
Example video demonstrating a CRT implant
Cost-effectiveness of CRT
Other Implantable Monitors
CardioMEMS is an implantable cardiac pulmonary arterial pressure monitor that sits within the pulmonary artery and measures dynamic information that may indicate early signs of worsening heart failure. This then transfer information to the physician and they can adjust medications as required5.
It has been shown to reduce hospitalisations for heart failure6.

Other benefits from Implantable Device Therapy
Implantable Electrical Cardiac Device (IECD) are very effective tools that offer both therapy and the ability to monitor patients in an outpatient setting. Many new devices have the abilities to then transmit important information such as therapy delivered, early signs of potential heart failure as well as regular maintenance information such as battery life, lead conditions etc. This is often referred to as “Remote Monitoring” ability of a implanted cardiac device.
This allows Cardiologists and other teams to monitor patients very closely for changes to their cardiac status in their own homes and be alerted to early changes that may require medical intervention8.
Examples of Remote Monitoring Devices


Left Ventricular Assist Device
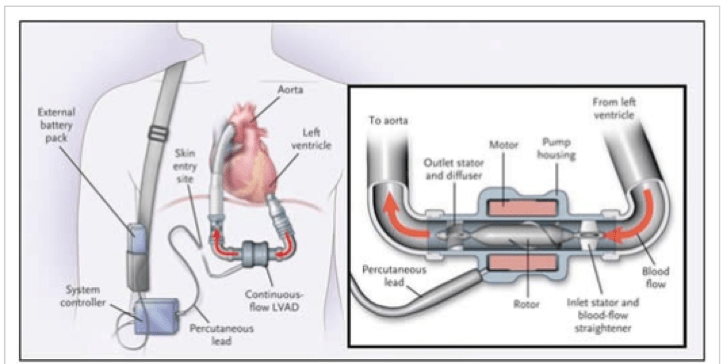
LVAD is a pump that can be used for patients in end stage heart failure. This therapy can also be used as a “bridge” whilst awaiting a potential heart transplant. In this therapy, the patient undergoes a surgical procedure where the LVAD assists the heart to pump blood to meet metabolic needs. The LVAD is attached to a portable battery pack so the patient may be able to move around (if clinically indicated).
Patient Disclaimer: All content on the Hope For Hearts site is created and published online for general information purposes only. It is not intended to be a substitute for professional medical advice and should not be relied on as health or personal advice. Please see your doctor if you have any questions or concerns.
Reference
- National Centre for Biotechnology Information
- Washington Heart Rhythm Associates
- American Heart Association
- Expert Review of Cardiovascular Therapy Journal
- National Centre for Biotechnology Information
- Abbott
- Abbott
- National Centre for Biotechnology Information
- Boston Scientific
- Abbott
- Biotronik
- Stanford Health Care
