Treatment Methods for Aortic Stenosis
Aortic valve replacement is regarded as the definitive therapy for severe aortic stenosis. The multi-disciplinary heart team will conduct a thorough evaluation of the patient’s status and make the final treatment decision for either surgical AVR (SAVR) or transcatheter aortic valve implantation (TAVI), which is a less invasive treatment compared to surgery. This decision will be made based on patient risk for surgery and suitability.1
Types of Treatment Options for Aortic Stenosis
There are three main surgical procedures for treating aortic stenosis:
- Surgical aortic valve replacement (SAVR)
- Transcatheter aortic valve implantation (TAVI)
- Balloon valvuloplasty.
“Severe aortic stenosis is a terminal mechanical condition, that very fortunately has a wonderful mechanical solution, which is an aortic valve replacement,” Interventional Cardiologist Associate Professor Dion Stub explains below. He further outlines the treatment options for severe aortic stenosis including surgical aortic valve replacement (SAVR), transcatheter aortic valve implantation (TAVI), and balloon valvuloplasty.
Types of Replacement Valves
Aortic valve replacement involves removing the diseased valve and replacing it with an artificial valve. There are two types of artificial valves:
- Biological (tissue) valves (commonly made out of pig tissue (porcine) or cow tissue (bovine), and
- Mechanical valves (made out of carbon fibre).
Mechanical valves are very durable and rarely fail. However, they may require anticoagulation such as warfarin, which increases the risk of bleeding and may require regular monitoring. On the other hand, biological valves do not require blood thinners although they may not last as long as mechanical valves2.
The average time a biological valve lasts is around 15-20 years, to which a patient may require another operation after this3. This is a complex decision that the patient must ultimately make and therefore, should discuss with their surgeon.

Image 1: Two types of artificial valves4
Cardiothoracic Surgeon Dr Jim Dimitriou and Interventional Cardiologist, Dr Sonny Palmer have a comprehensive discussion about the treatment of aortic stenosis. They cover what the studies and trials say about TAVI, how the age and risk level of a patient can influence their treatment, why people aren’t receiving treatment, and the future of aortic stenosis.
Surgical Aortic Valve Replacement (SAVR)
Surgical aortic valve replacement is a treatment option for aortic stenosis.
Surgical aortic valve replacement is an open heart procedure, where the sternum is divided to visualise the heart. Once the heart is accessed, patients may be put on a heart-lung machine for the duration of the procedure, while cardiac surgeons replace or repair the aortic valve. At this time the surgeon may also perform other procedures if needed, such as coronary artery bypass grafting, to avoid the patient requiring an additional operation.
Cardiothoracic Surgeon Dr Jim Dimitriou explains the difference between the surgical aortic valve replacement (SAVR) and transcatheter aortic valve implantation (TAVI). Further explaining the considerations for age and use of warfarin, and the importance of the structural heart team, “in the general management of the patient, the best way forward is not to think of it as your procedure or my procedure, but the management of aortic stenosis.”
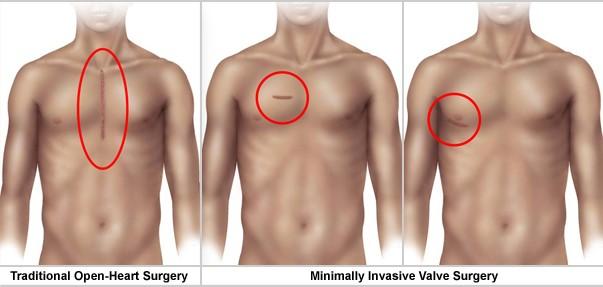
Image 2: Surgical approaches5
In some cases of Aortic Stenosis, there may also be an associated need to replace a portion of the aorta and the aortic valve. This is called a “Bentall’s Procedure” and replaces the aortic valve and the aortic arch with a manufactured graft that replaces the diseased aorta. The aortic valve may be replaced by a new valve that may be made of either biological material (porcine or bovine) or a metal valve (usually cobalt). Cardiothoracic Surgeon, Dr George Matalanis, explains what materials are used in the Bentall’s Procedure in the below video.
Recovery Period
Patients will often spend a few days within the intensive care unit (ICU) for close monitoring. Once the patient is ready to leave the ICU, they transition to the ward for monitoring until the surgical team decides the patient is fit for discharge home. A full recovery can usually take up to 8 weeks, although individual recovery times can vary. Most patients are able to drive in about 3 to 8 weeks after surgery. The surgical team will provide specific guidelines regarding recovery6.
The TAVI Procedure
In a TAVI procedure, a biological (tissue) valve is mounted inside a stent (a circular wire mesh). The stent is then compressed so that it can fit inside a small delivery sheath (tube). The TAVI valve is then delivered to the aortic valve, the stent is expanded, and the biological valve inside begins to work. In TAVI the calcified leaflets of the patient’s diseased aortic valve are not removed; instead, they are pushed to the side when the stent expands and help to lock the stent in place.
Dr Matthew Brooks, Interventional Cardiologist, discusses the improvements the percutaneous treatment option, transcatheter aortic valve implantation (TAVI) has had for the treatment of aortic stenosis. In Australia, typically a TAVI can now be performed under local anesthetic and can be as short as 40 minutes. “It’s minimally invasive, and the results from the procedure are tremendous in terms of valve function and the complication rate is very low.”
There are multiple ways of delivering the TAVI valve to the aortic valve position including:
- Transfemoral – The delivery sheath is inserted into the femoral artery in the patient’s groin, and the TAVI valve travels upwards through the artery to the aortic valve.
- Transapical – A 5-10cm horizontal incision is made on the left side of the chest below the nipple line, which provides direct access to the heart. The delivery sheath is then inserted in the apex of the heart and the TAVI valve inserted.
- Transaortic – A small incision at the top of the sternum (breast bone) is made and that the delivery sheath is inserted into the aorta (the large blood vessel that the aortic valve is in).7
The Transcatheter Aortic Valve Implantation (TAVI) procedure is explained in detail in the below video, narrated by Dr Alex Willson, Interventional Cardiologist. Commonly performed from the femoral artery, a large sheath is inserted and a wire is placed across the aortic valve positioned within the left ventricle. The transcatheter valve is positioned within the abdominal aorta, it is then advanced across the aortic arch and positioned across the aortic valve. Once the position is accurate the balloon is deflated which deploys the transcatheter valve.
TAVI Procedure: Step-By-Step
 Step 1 of 4
Step 1 of 4
A small incision is made into the Femoral Artery in your groin. Then a sheath is introduced into the artery and a long radiopaque wire is inserted into the sheath, this will sit just superior to the aorta. This allows the introduction of a larger sheath which will deliver the new aortic valve.
 Step 2 of 4
Step 2 of 4
The new aortic valve is placed on a delivery sheath, compressed and made small enough to be delivered through the catheters already in the femoral artery.
 Step 3 of 4
Step 3 of 4
The radiopaque guidewire is introduced into the heart, and the delivery sheath is placed in position within the diseased native aortic valve. A balloon is inflated to increase the size of the native valve, and then a new valve is deployed within the old diseased valve. The catheters are then removed from the femoral artery.
 Step 4 of 4
Step 4 of 4
The new valve will begin working as soon as the catheters and wires are removed from the heart. Echocardiography testing during the procedure ensures that your new valve is functioning as effectively as it should. The femoral artery may be closed to prevent bruising and bleeding at the site.
The Complications of TAVI
“Unfortunately, there will never be a way to replace someone’s heart valve without any risk at all, but similarly the risks are very low and very acceptable,” Interventional Cardiologist, Dr Ronen Gurvitch explains the possible risks associated with transcatheter aortic valve implantation (TAVI). This Includes the common risks such as bruising or discomfort around the incision area, permanent pacemaker, and a very small risk of potential stroke or needing to convert to open heart surgery.
Balloon Valvuloplasty
Balloon aortic valvuloplasty is a treatment option for severe, symptomatic aortic stenosis. During this procedure, a balloon is inflated within the damaged aortic valve with the aim to increase the size of the valve, therefore relieving symptoms temporarily. Balloon aortic valvuloplasty may be done prior to a formal Transcatheter Aortic Valve Implantation (TAVI) procedure to assess the therapeutic response of a patient before performing the formal TAVI procedure.
Balloon Valvuloplasty is a procedure “that is not a cure or fix of the aortic valve, although we can provide relief of the aortic stenosis for a period of time,” says Interventional Cardiologist, Dr Alex Willson. He further notes in the above video that this procedure is typically reserved for high risk or frail patients, as a bridge to further treatment, or in the assessment of how the patients will respond to treatment.
The treatment is considered temporary only, as the damaged valve will likely return to its previous state over time. It has emerged that restenosis and recurrence of symptoms are often seen in as little as 6 months post balloon valvuloplasty. The goal for this treatment is to try to reduce the transaortic valvular pressure gradient by as much as 50 mmHg.8 The patient may see a return of symptoms such as heart failure and other signs of aortic stenosis rapidly due to the severity of the diseased valve.
This percutaneous procedure is carried out in a Cardiac Catheter Lab and is often considered a palliative option for those patients deemed not suitable for other cardiac procedures, due to intraoperative surgical risk or other factors. Balloon aortic valvuloplasty may also be used as a bridge to aortic valve repair or replacement while a patient recovers sufficient physical strength to sustain a more formal TAVI or surgical aortic valve replacement.9
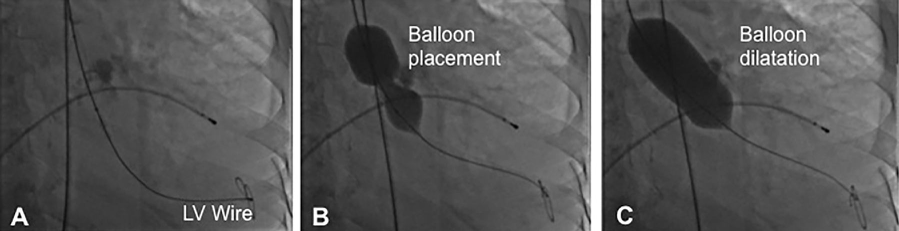
Image 1: Example of a Balloon Valvuloplasty procedure
