Treatment for Bradycardia
Patients who have been identified to have slow heart rates may undergo a variety of treatments. These may typically include either stopping or changing medications that may have been causing the slow heart rate or undergoing implantation of a permanent pacemaker.
Additionally, sleep apnoea treatment may help in reducing symptoms and in the case of electrolyte imbalances or hormonal deficiencies, these can be addressed with medication which in turn can relieve the bradycardia.
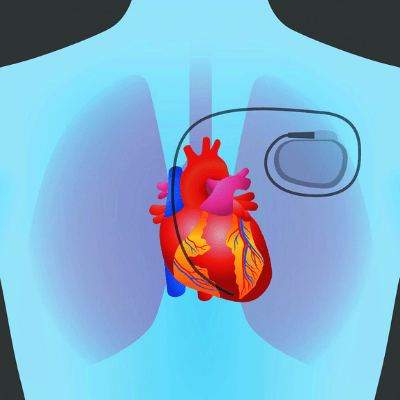
For patients with electrical abnormalities, typically the most appropriate treatment method is the implantation of a permanent pacemaker. A pacemaker will typically include a lead (or multiple leads) that are implanted within your heart and connected to a pacemaker unit (where the battery and electrical components are). A pacemaker can monitor the heart rate for natural activity and then “stimulate” the heart to contract or beat when it detects abnormal activity, essentially mimicking the natural electrical conduction of the heart.
How do permanent pacemakers work?
Below is a video explaining how permanent pacemakers work by identifying an abnormal heart rhythm and in turn stimulating the heart to return to its normal rhythm.
Video Source: Biotronik
Are there different types of permanent pacemakers?
There are three types of traditional pacemakers that are used in adults. These include:
- Single chamber pacemaker,
- Dual-chamber pacemaker, and
- Biventricular pacemaker.
However, the type of pacemaker will depend on the individual patients’ circumstances. Below is a detailed description of these three types of pacemakers along with two other types: leadless and cardiac resynchronisation therapy (CRT) pacemakers.
Single chamber pacemaker: Where a single lead is inserted into the right ventricle and is often used in the case of a patient with bradycardia and underlying atrial fibrillation (AF).
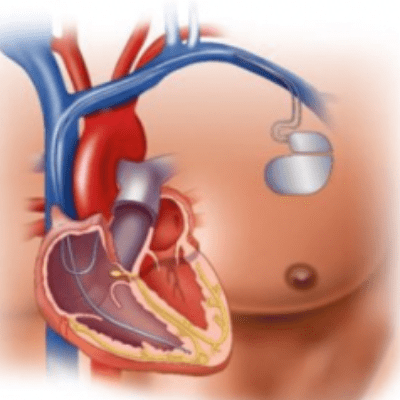
Dual-chamber pacemaker: have two leads implanted into the heart, one positioned in the right ventricle and the other in the right atrium.
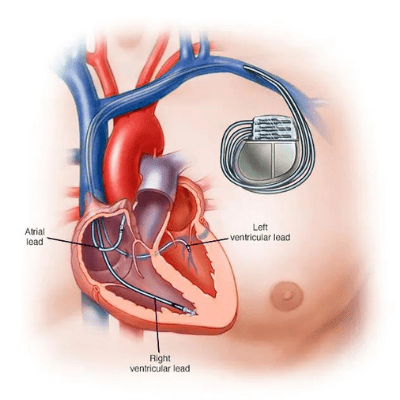
Biventricular pacemakers: are used in those patients with heart failure who may also have electrical conduction disease. It has three leads implanted, one in the atrium, the right ventricle, and one that sits over the left ventricle. The aim of these pacemakers is to increase the pumping mechanism of the heart by synchronising the right and left ventricles to improve ventricular contraction, which in turn improve the pumping action of the heart.
Leadless Pacemakers: this type of pacemaker has no leads and the device is essentially “screwed” into the inner lining of the ventricle. The device is implanted through the femoral artery (in the groin) and a catheter delivers the leadless pacemaker to the heart, where it is screwed into the ventricle. Following this, the catheters are removed leaving the pacemaker positioned within the heart and working as normal. This pacemaker device functions the same as the above pacemakers with all of the same functions as one that is implanted on the chest with lead(s) attached.
Below is a video animation of a leadless pacemaker implant.
Please note this is one example of this device and there may be other products available in your region.
Cardiac Resynchronisation Therapy (CRT) Pacemakers
In patients who have a slow heart rate and require pacemaker implantation, some may receive a Cardiac Resynchronisation Therapy (CRT) pacemaker. These devices are specifically used for people who have also been diagnosed with heart failure. A CRT pacemaker aims to “re-synchronise” the left and right ventricles, to improve cardiac function. A third lead is implanted and works to “re-synchronise” both ventricles to work together and improve cardiac output.
Not all patients are suitable for these devices and the patients’ personal Cardiology team will be able to decide if this is the right pacemaker for the individual.
