About Atrial Fibrillation
Atrial fibrillation (AF) is a common heart arrhythmia where the electrical signals that stimulate the atria (upper chambers) move from being a coordinated organised electrical pattern to a chaotically, disorganised electrical pattern resulting in symptoms such as:
- Shortness of breath,
- Palpitations or racing or fluttering feeling in the chest,
- Decreased exercise tolerance,
- Fatigue,
- Lightheadedness,
- Chest pain, and
- Signs of heart failure (swollen feet, breathlessness and decreased exercise tolerance)1.
It is estimated that there are approximately 330,000 people in Australia who may suffer from AF, however, this incidence may be rising due to the increase in risk factors such as obesity and the growing prevalence of Type 2 Diabetes Mellitus within our communities, coupled with the increasing age of our population.
It is probable that these numbers are underrepresented as many patients with AF may not have any signs or symptoms of the condition. It is thought that up to 30% of patients with AF may not have symptoms, which can make both diagnosis and treatment of AF a challenge3.
Diagnosis of Atrial Fibrillation
Atrial fibrillation may be suspected due to symptoms by simply taking the patients radial pulse and noting an “irregular” pattern in the heart rate through palpation. A more formal diagnosis can be made via an Electrocardiograph or “ECG” which will demonstrate the irregular heart rate.
Depending on the type of AF, other methods may be required. These may include ambulatory ECG monitors which can be used for a variety of periods ranging from 24 hours, up to several days. This information is then reviewed by a Cardiology team to confirm the diagnosis4.
Quality of Life Impact of Atrial Fibrillation
Atrial fibrillation is a common and sustained arrhythmia that increases with age, with as many as 7 in 10 patients over the age of 65 – 85 years old being affected by AF. Due to the complexity surrounding patients with multiple medical conditions in this age group, AF may cause a direct reduction in the cardiac output, therefore, impacting on the ability to perform many tasks around the home. As an example, this may present as a reduction in exercise capacity or an inability to walk to the shops to obtain regular groceries. This may lead to social isolation and have an impact on the mental health of patients and their supporting networks as an increased level of support may be required5.
Economic Cost of Atrial Fibrillation
The financial impact of Atrial Fibrillation has been estimated to cost approx $6.6B US Dollars, which includes treatment, frequent presentations and hospitalisations and also medications to treat these complicated patients. It must be remembered that many patients in the age group for AF may have many other health conditions that may either exacerbate symptoms or other complications of their underlying illnesses. These are important factors to keep in mind when considering the overall costs associated with AF6.
Causes of Atrial Fibrillation
While there are no specific known causes of AF, there are a number of predisposing heart conditions that may increase the risk of AF:
- Hypertension,
- Artherosclerosis,
- Heart valve disease,
- Cardiomyopathy,
- Some congenital heart conditions.
It is often present in patients with other comorbidities and conditions including:
- Diabetes,
- Obesity,
- Chronic obstructive pulmonary disease (such as emphysema),
- Sleep apnoea,
- Pulmonary embolus,
- Endocrine disorders such as overactive thyroid gland.
It has been documented that AF may occur in patients who have the following lifestyle triggers:
- Alcohol binge drinking,
- High intake of caffeine, tea, and energy drinks,
- Smoking,
- Methamphetamines and cocaine ingestion7.
Risks of Atrial Fibrillation
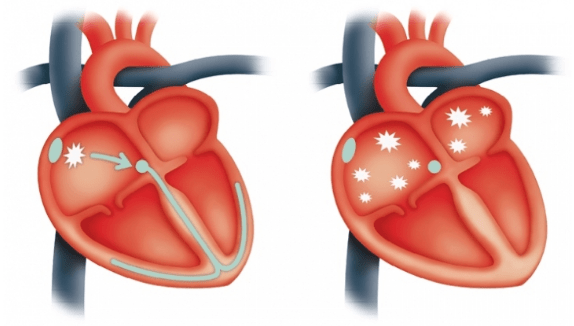
Atrial fibrillation causes an irregular heartbeat and may lead to the formation of small blood clots that can sit within a patient’s heart. These formed blood clots may then be pumped from the heart and lodge in smaller blood vessels anywhere in the body, including the brain and lungs.
These small clots may cause small or large strokes in some patients. It is estimated that patients with AF may have a significant increase in the risk of stroke due to the formation of blood clots. This may be reduced by the commencement of a blood-thinning agent (anti-coagulant) to reduce clot formation, however, anticoagulation can increase bleeding risks and will need to be considered as part of a comprehensive medical assessment8.
An irregular heartbeat may also affect the capacity of the heart to meet the metabolic demands due to a reduction in cardiac output, which may then lead to poor exercise tolerance, an increased risk of heart failure and other complications. Patients with AF have been associated with a higher risk of stroke, heart failure and death9.
Types of Atrial Fibrillation
There are three recognised types of Atrial Fibrillation:
- Paroxysmal AF – Typically occurs then stops without any treatment, usually with the heart returning to a normal, coordinated electrical signal from the atria. This may last seconds to hours or days. This type of AF may be characterised with an irregular pulse and potentially some symptoms such as palpitations as well.
- Persistent AF – Usually characterised as AF requiring some form of intervention to end the irregular heartbeat and symptoms. This treatment may consist of simple medication of require an “electrical reset” by the use of a defibrillator to rest the hearts electrical system and is known as a Cardioversion.
- Long-standing Persistent AF – A new classification previously known as permanent AF, this type of AF may be resistant to treatment and is likely a permanent heart rhythm10.
Origins of Atrial Fibrillation
The actual cause of Atrial Fibrillation is not well understood and is likely a complex mechanism, involving several factors. AF is thought to originate within the left atrium near the pulmonary veins, and it may be from one or many focal areas of activity within the left atrium. A large or dilated left atrium is also thought to be a risk factor for AF11.
Patients with structural heart disease (such as hypertension and cardiac valve disorders) and other abnormalities may also lead to an increased risk of AF, however, AF is still seen in many patients who don’t have structural heart disease12.
To learn about the treatment of Atrial Fibrillation, click here.
