About Atrial Flutter
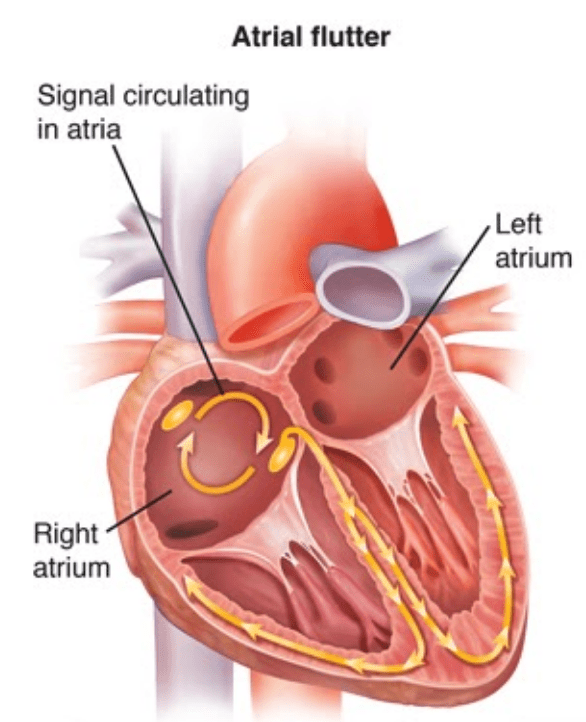
Atrial flutter (AFL) is the second most common heart arrhythmia and is similar to Atrial Fibrillation (AF) in that ALF can cause a rapid heartbeat. AFL can also result in symptoms similar to AF, but unlike AF where the electrical stimuli are irregular and chaotic, AFL is characterised by an organised abnormal circuit within the right side of the atria.
Many of these organised electrical signals are then conducted to the ventricles, which in turn cause the rapid heartbeat. This can result in heart rates of greater than 150 bpm.1
Risk Factors for Atrial Flutter
Age is suspected to be one of the most significant risk factors. Atrial flutter is most commonly seen in patients over the age of 50; however, this condition can be found in patients of all ages. The presence of other medical conditions can increase the risk of AFL:
- Heart attack,
- Diabetes,
- Heart failure,
- Previous congenital heart disease/surgery,
- Binge alcohol drinking,
- Chronic lung diseases,
- Structural heart diseases (such as aortic stenosis),
- Thyroid dysfunction,
- Obstructive sleep apnoea,
- Cardiac preexcitation syndromes, such as Wolff Parkinson White syndrome.3
Signs and Symptoms of Atrial Flutter
Patients with Atrial Flutter can present with many similarities to those with Atrial Fibrillation (AF), such as:
- Syncope,
- Heart failure,
- Palpitations or irregular heartbeat,
- Dyspnoea or shortness of breath,
- Chest pain,
- “Flutter” feeling in the throat and/or chest,
- Stroke – however, less likely to occur in AFL when compared to AF, but is possible if blood clots are present.4
Diagnosis of Atrial Flutter
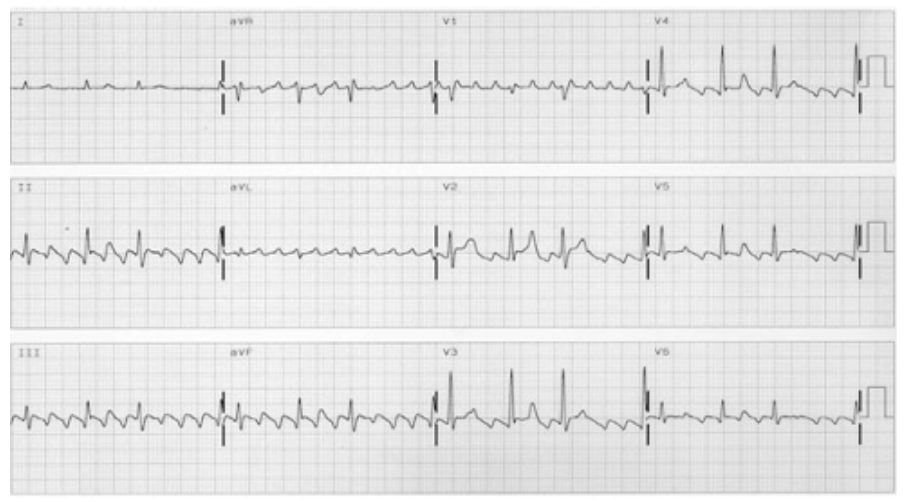
The diagnosis of atrial flutter (AFL) is usually on a surface Electrocardiograph (ECG) after presenting with symptoms. It is characterised by a rapid atrial signal with either a regular or irregular ventricular contraction, usually at fast heart rates which is often around 150 bpm. This means the heartbeat is likely to be regular, but an AFL is known to have a variable conduction pattern through the atrio-ventricular node and can result in an irregular pulse.
There are two recognised types of AFL:
- Typical AFL – is commonly an organised arrhythmia that is caused by an electrical loop pathway within the right atria. The heart rate may be irregular due to the intermittent conduction (through the atrio-ventricular node) of the signal to stimulate the ventricles to contract, hence an irregular (but rapid) heartbeat. On the below ECG, it is characterised by a “sawtooth” pattern.
- Atypical AFL – is very similar in clinical presentation though the organised electrical stimulus may arise within multiple regions within or near the right atria. Again, this type of surface ECG may present very similarly to the typical AFL, demonstrating as a “sawtooth” pattern of electrical stimuli.
A surface ECG may look like:
An echocardiogram can be a useful tool in the identification of any structural heart abnormalities that may precipitate AFL. It’s helpful to understand the pumping effectiveness of the heart, also called the “ejection fraction”, which can be a direct measure of cardiac function.
Electrolyte / endocrine function tests are an important determining factor in the diagnosis of AFL.
Treatment of Atrial Flutter
Medical Management for Atrial Flutter
The medical goals for the treatment of AFL are similar to that of Atrial Fibrillation (AF), which is:
- Heart rate control,
- Rhythm control, and
- Prevention of thromboemboli (blood clots).
These are typically achieved through medication administration and close monitoring by a local doctor and cardiologist. A patients’ local physician should monitor for adverse reactions to these medications (such as fatigue, fainting and lethargy amongst others signs) as not all medications may be well tolerated and it could take some time to find the best regime for each patient.
Lifestyle factors and other medical conditions that may increase the risk for AFL should be addressed by the patient in conjunction with close medical supervision. These factors may include:
- Hypothyroidism / endocrine disorders,
- Alcohol / drug abuse,
- Obesity,
- Caffeine intake.
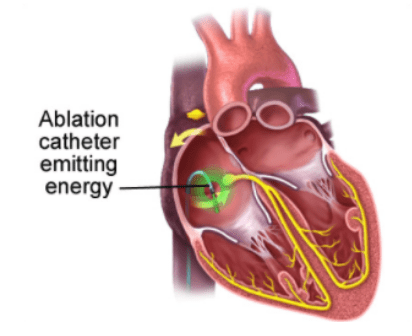
Procedural Catheter Based Therapy for Atrial Flutter
Persistent AFL that causes significant symptoms or impact on quality of life may be treated by a Catheter Radiofrequency Ablation. This procedure, commonly referred to as atrial flutter ablation, is where several electrical catheters are inserted into the right side of the atria via the groin and the “abnormal circuit” is altered through the application of either radiofrequency heat or cryotherapy to stop the “abnormal electrical pathway.”
This procedure can have a high level of success, and in some cases, might be considered a first-line treatment for AFL. This procedure has shown to be effective in controlling both types of AFL but can also be complicated depending on the patients’ anatomy and risk factors.6
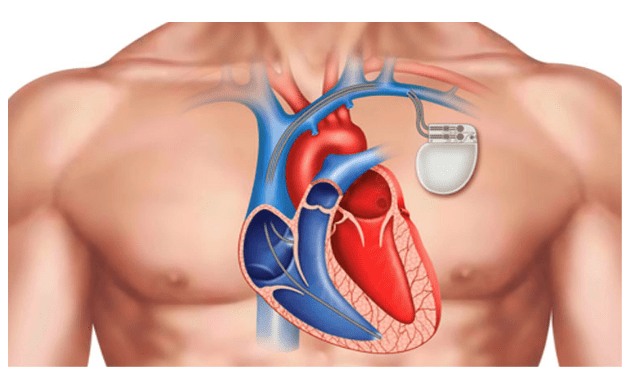
In those cases where AFL ablation is not effective, some patients may elect to undergo a procedure where the “bridge” (also known as the atrioventricular node or AV node) between the atria and the ventricle is ablated (or altered) in a similar fashion to a typical AFL ablation.
This often results in the atria and the ventricles essentially being electrically disconnected from each other and a permanent pacemaker is implanted to help the heart modulate appropriate heart rates. This procedure is often permanent and will require either one or two leads, depending on the individual patients’ circumstances. In some cases, where the patient is known to have heart failure, a Cardiac Resynchronisation Device may be implanted.