Many patients may be referred for a pacemaker or an implantable defibrillator for a variety of reasons by their Cardiologist, Electrophysiologist or Cardiac Surgeon. This article will shed some light on why you may be referred for consideration of a device and how it may benefit you.
What are pacemakers?
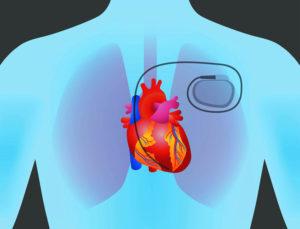
Pacemakers are small electronic devices that may consist of an electrical wire that is placed inside the heart and attached to an electronic device with a battery, that stimulates this wire to create a heart beat. The main reason that patients may need a pacemaker is that there has been an electrical dysfunction within the electrical system in the heart, resulting in a very slow heart rate. A slow heart rate is often called bradycardia where the ventricular rate is slow enough that a patient may become dizzy or syncopal.1
There are three types of pacemakers currently used for patients with bradycardia:
A Single-Chamber Pacemaker is used if the patient has an underlying heart rhythm called Atrial Fibrillation, and periods of very slow rates leading to a dizzy or syncopal episode. A small, single electrical lead will be implanted in the right ventricle and the lead is connected to the pacemaker (containing a battery and electronic circuitry). This pacemaker will stimulate the lead which in turn will stimulate the heart muscle to contract, and ultimately increase your heart rate.
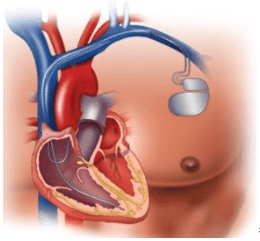
Dual-Chamber Pacemakers are used in patients with bradycardia (slow heart rate) who do not have atrial fibrillation or atrial flutter as the predominant heart rhythm. This involves two small electrical leads, one implanted in the right atrium and the other in the right ventricle which are then connected to a pacemaker (containing the battery and electronic circuitry). This pacemaker will stimulate the leads to produce a coordinated heart rhythm.
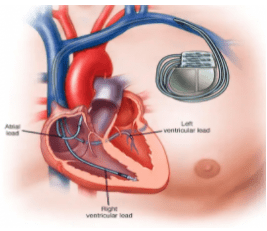
A third pacemaker option is a Biventricular Pacemaker, used in patients with significant heart failure or cardiomyopathies. These devices have three leads, one in the right atrium, a second in the right ventricle and a third sits over the left ventricle. This type of cardiac device aims to improve cardiac function by “synchronising” the right and left ventricles to contract “together” and improve the strength and volume of blood ejected from the ventricles.
Implantable Cardioverter Defibrillators (ICD) are used to detect and treat ventricular arrhythmias, sudden cardiac arrest and may also be used for those patients with heart failure. They may be referred to as single-chamber, dual-chamber or biventricular Cardiac Resynchronisation Therapy (BIV ICD), which refers to a third lead used to resynchronise the right and left ventricles.
These devices have a similar function to pacemakers as they can pace the heart to prevent slow heart rates, but also deliver a high energy shock aimed at disrupting a lethal arrhythmia when detected by the device. They may have one or two leads placed in a similar position to leads in pacemakers, but the ventricular lead is larger and may have “coils” to deliver this high energy to the majority of the heart.2
A newer type of defibrillator is called a Subcutaneous Defibrillator or Sub Q ICD. This technology implants the lead, that delivers the shock, in the subcutaneous tissue in the chest (not in the heart itself) and is attached to a defibrillator (battery and electronic circuitry) that senses the arrhythmia and delivers a shock to revert the heart to a normal rhythm.
These complex devices may also have inbuilt alarms to detect arrhythmias such as atrial fibrillation or early signs of heart failure (amongst other conditions) and relay this information to Cardiology teams for early intervention. This information may be shared with your Cardiology team online with secure messaging services to maintain your privacy, which can be referred to as “home monitoring.” Your individual Cardiology team will advise you about any special features that may be relevant to your treatment.
Written by Shane Bassett, Clinical Content Director, Connect The Docs, RN/BN/CCRN
Image Credit: HealthBeat. The following image is of George Burhance, a retired industrial electrician who had a biventricular pacemaker implanted due to having an irregular heart rhythm. To read about his success story please click the link.
All information contained in this article has been derived from Hope For Hearts, cardiac resource centre.
To find a General Practitioner (GP) or a Cardiologist near you, visit www.hopeforhearts.com.au/specialists

