About Long QT Syndrome
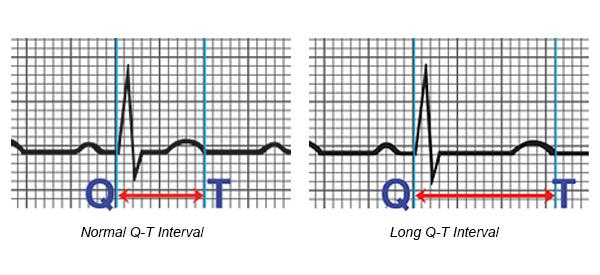
Long QT syndrome (LQTS) is a genetically inherited arrhythmia disorder where the heart may develop sudden and dangerous Ventricular rhythms. LQTS is characterised by a prolonged QT interval at baseline.
In many cases, long QT syndrome is an inherited syndrome but can be caused by medications that affect electrical conduction within the heart. The disorder has the capacity to initiate ventricular tachyarrhythmias (such as Torsade de Pointe or Ventricular Fibrillation) that may lead to syncope (fainting), cardiac arrest and death.
Prevalence of Long QT Syndrome
The actual incidence of LQTS is not clear and has been estimated to 1:2000 lives births in one study of 44,500 neonates. LQTS has been shown to be shared equally amongst males and females.1
Signs and symptoms of Long QT Syndrome
LQTS is often diagnosed after the sudden death of a family member, particularly at a young age, however, can also be picked up routinely on an Electrocardiograph (ECG). Any survivor of a cardiac arrest should be investigated for LQTS in the absence of mitigating circumstances, such as no myocardial infarction. A syncopal event whilst exercising should also be a red flag for LQTS.
Depending on the genetic mutation, these cardiac events may be precipitated by:
- Exercise,
- Severe emotional response,
- Sudden exposure to very cold temperatures, and
- Swimming.
Any patients that are presenting post these events should be screened for LQTS as a matter of urgency.
Patients with deranged electrolytes (such as sodium, potassium, magnesium) should also have routine ECG to determine if the QT interval has been affected by abnormal levels of these electrolytes.
Patients who have no history of cardiac causes should be investigated to determine if an interaction between prescribed (or otherwise) medication may have lead to a prolongation of the QT interval.2
Diagnosis of Long QT Syndrome
Routine 12 lead Electrocardiograph (ECG) will show a prolonged QT interval and the use of Holter monitors may allow a longer range of ambulatory ECG. Additionally, imaging studies (echocardiography/ MRI) can identify other potential causes of LQTS, such as hypertrophic cardiomyopathy (HOCM) which could also predispose a patient to LQTS.
As mentioned earlier, it’s important to also note medication that the patient may be taking and consider if this has the potential to alter the QT interval as a side effect or therapeutic adjunct to other medical conditions.
Depending on the genetic variant of LQTS, a 12 lead ECG may present with a number of subtle changes involving the QT interval, however, a QT interval of > 450 ms is considered abnormal.
Treatment for Long QT Syndrome
Medical Management
For those patients who had LQTS as a result of medications that have increased their QT, these medications should be avoided or monitored closely if unavoidable. Patients with a genetic component causing LQTS can use medications that block some of the autonomic response to stressors which may reduce the incidence of a future cardiac event.
Procedural Management
Patients with LQTS who have survived a cardiac event, or have a strong familial history may be offered an Implantable Cardioverter Defibrillator (ICD). These devices are useful if the patient has a spontaneous ventricular arrhythmia, as the device can sense, detect and treat the arrhythmia with a series of high voltage “shocks” to reset the normal electrical activation of the heart and provide back up pacemaker support if required.4
