About Wolff-Parkinson-White Syndrome
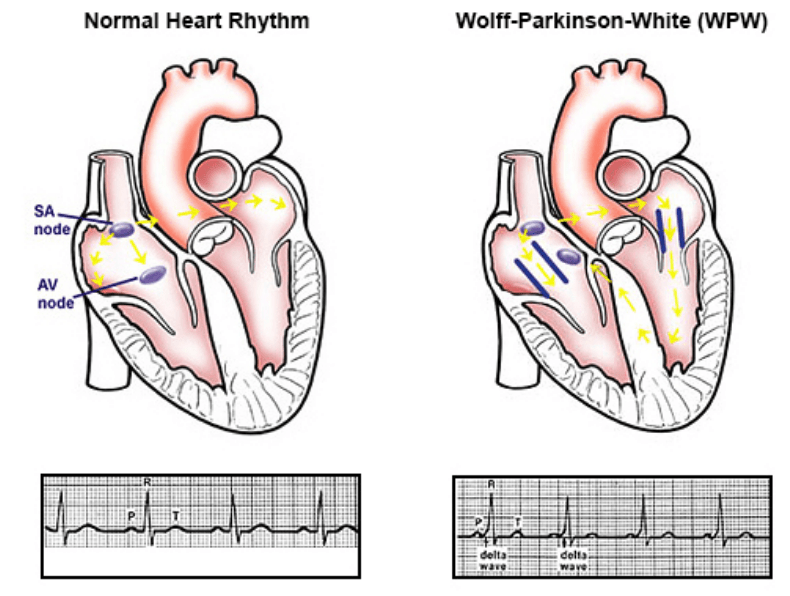
Wolff-Parkinson-White Syndrome (WPW) is an arrhythmia that may be characterised by abnormal electrical pathways that lead to very rapid heart rates. Patients with WPW may have an accessory electrical pathway (circuit) that allows normal electrical signals from the atrium to bypass the bridge (Atrioventricular node AV node) between the upper and lower chambers. This creates a “loop circuit” which results in rapid heart rates.
The AV nodes’ role is to limit the heart rate, by slowing down the stimulation from the atria. Therefore, the aberrant pathway allows these abnormal electrical pulses to bypass the AV node, stimulating ventricular contraction, and ensuring rapid heart rates. WPW forms a class of arrhythmias known as Paroxysmal supraventricular tachycardia (SVT).
WPW may also occur in patients who may have other structural heart abnormalities such as Epstein anomaly that can affect the tricuspid valve, which in turn, affects blood flow from the Right atrium to the Right Ventricle.1
What is Wolff-Parkinson-White Syndrome?
In the below video, Cardiologist Electrophysiologist Dr Tchou, explains a heart arrhythmia, Wolff-Parkinson-White Syndrome.
Prevalence of Wolff-Parkinson-White (WPW) Syndrome
WPW can occur at any age and is thought to affect approximately 1-3 per 1000 patients. The cause of WPW is unknown in the majority of cases, however, it is thought that a small percentage of these patients may have a genetic mutation. Many cases of WPW are not inherited with little to no family history. In patients who have familial WPW syndrome, the patient will have inherited the condition from an affected parent.3
Signs and symptoms of Wolff-Parkinson-White (WPW) Syndrome
Patients with WPW may present with the following signs or symptoms:
- Rapid heart rates,
- Palpitations,
- Shortness of breath,
- “Fluttering” feeling in throat,
- Low blood pressure,
- Dizziness / Syncope, or
- Cardiac Arrest (rare).4
Diagnosis of Wolff-Parkinson-White (WPW) Syndrome
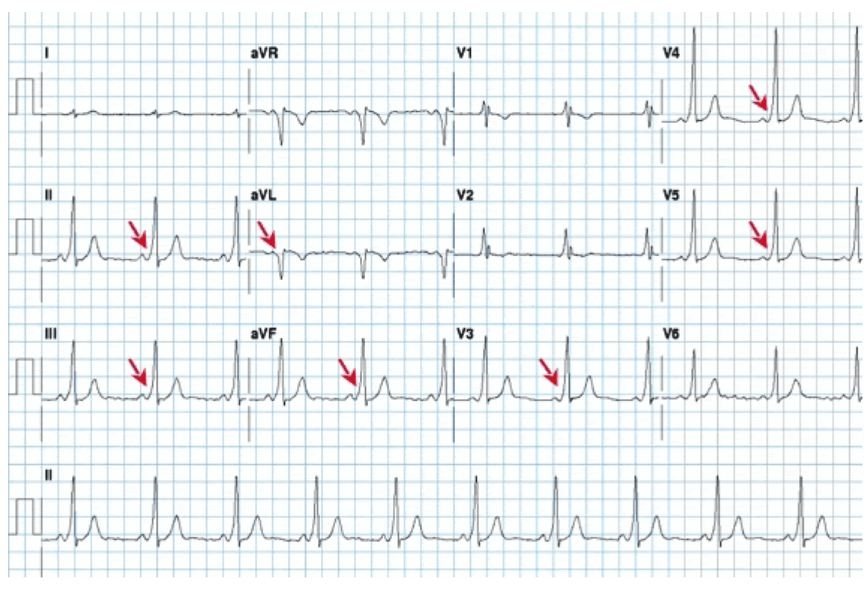
A formal diagnosis of WPW can only be made after an Electrocardiogram (ECG) that demonstrates changes on a surface ECG and indicates the potential for a “pre-excitation” syndrome. It is not uncommon for patients who have no symptoms of the condition to be diagnosed with WPW after a routine ECG that may highlight specific changes on the ECG. The presence of a “delta wave” on an ECG may indicate WPW as a clinical diagnosis.5
A Delta wave may also be described as a “slurring” of the QRS complex on ECG as highlighted with red arrows below:
More commonly, patients will present with symptoms and the condition is diagnosed after a review of their ECG. A more formal medical history might ask more detailed questions to elicit if the patient has had any previous symptoms of the condition such as:
- Fainting episodes,
- Palpitations,
- The sudden death of people in your family, or
- Any history of other arrhythmias such as Atrial Fibrillation.7
Treatment of Wolff-Parkinson-White (WPW) Syndrome
Treatment for WPW may depend on the presence of other structural heart conditions, frequency of symptoms such as syncope (dizziness) and other familial histories, if relevant.
There are three main treatment options:
- Monitoring – If the patient has no or very infrequent symptoms their Cardiologist may recommend this option. The patients’ Cardiology team will decide the relative risk of this action in relation to the patients’ individual circumstances.
- Medication – There are many medications that can help to prevent symptoms, though not all will be effective or well-tolerated. A Cardiology team will decide which is the most appropriate medication to take and review the effectiveness of this medication on a case by case basis.
- Catheter Ablation – The goal of catheter ablation is to disrupt or alter the capacity for the alternative circuit or “pathway” to facilitate rapid heart rates. This may be performed using Radiofrequency ablation (heat) or Cryoablation (cold) to destroy the area of excitation, and ultimately stopping the potential for WPW recurring.8
