Medical Treatment of Atrial Fibrillation
The therapeutic goals of Atrial Fibrillation (AF) can be divided into three common goals:
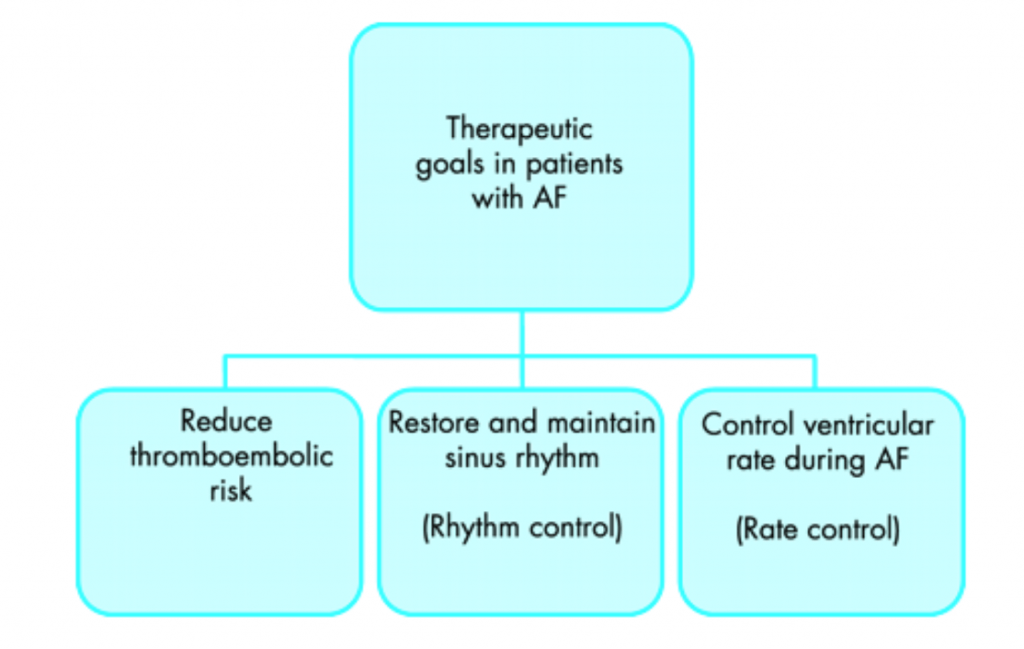
Thromboembolic Risk
The goal is to reduce the risk of blood clots that can form when patients have an irregular heartbeat and make their way to other parts of the body. These clots can potentially lodge in small blood vessels within the brain, lungs and other structures. Initiation of this therapy will also include a risk assessment of overall bleeding potential, taking into account factors such as cardiovascular risks (including structural heart disease and ischaemic heart disease), diabetes, age and overall health of the individual patient2.
Rhythm Control
This refers to the preferred rhythm known as “normal sinus rhythm”, which is when the electrical system of the heart follows the normal pathway and the heartbeat is, in essence, regular, not irregular as characterised by Atrial Fibrillation (AF). Many patients may have symptoms such as palpitations, shortness of breath and poor exercise tolerance when in AF. These symptoms are obvious to many patients, but not all may be aware of the irregular heart rhythm3.
Many medications are available that aim to reduce the irritability of the heart that may precipitate an episode of AF. These medications attempt to promote normal electrical activity and therefore maintain normal sinus rhythm. However, these medications may also have side effects and can have an effect on underlying medical conditions. These treatment goals need to be individualised and based on each patient’s overall risk factors as determined by the medical team4.
Rate Control
Rate control goals refer to keeping the underlying heart rate (beats per minute) under control during an episode of Atrial Fibrillation (AF). While there is no such number as an optimal heart rate for patients with AF, suggested hearts rates generally relate to a target heart rate at rest and another target when a patient is exercising5.
Regular review of medications used for rate control may be required to ensure that patients with AF are able to meet their activities of daily living such as housework and exercise. The underlying goal must also balance between having a heart rate so low, that patients are not able to perform the activities required for daily living6.
Procedural Management of Atrial Fibrillation
There are many patients with symptomatic Atrial Fibrillation (AF) who are unable to tolerate medication due to the side effects or patients with severe symptoms of AF where medical management may no longer be an ongoing option due to the impact on lifestyle. Atrial Fibrillation ablation may be a treatment to help manage AF.
There are two main types of energy used to ablate the myocardium to treat AF:
- Radiofrequency ablation
- Cryotherapy ablation
AF ablation is a catheter-based therapy usually performed in a Cardiac Catheter Lab (CCL) where small electrical catheters are passed through large vessels in the groin and moved into the heart, where a stimulus / therapeutic modality aims to ablate or alter the abnormal electrical pathways that are thought to be responsible for AF.
The procedure aims to isolate the electrical stimulus within the atria that may cause AF and prevent these abnormal electrical stimuli from initiating further episodes of AF. However, this type of treatment is not suitable for all patients with AF and a patient’s Cardiologist will be best suited to explore individualised treatment options7.
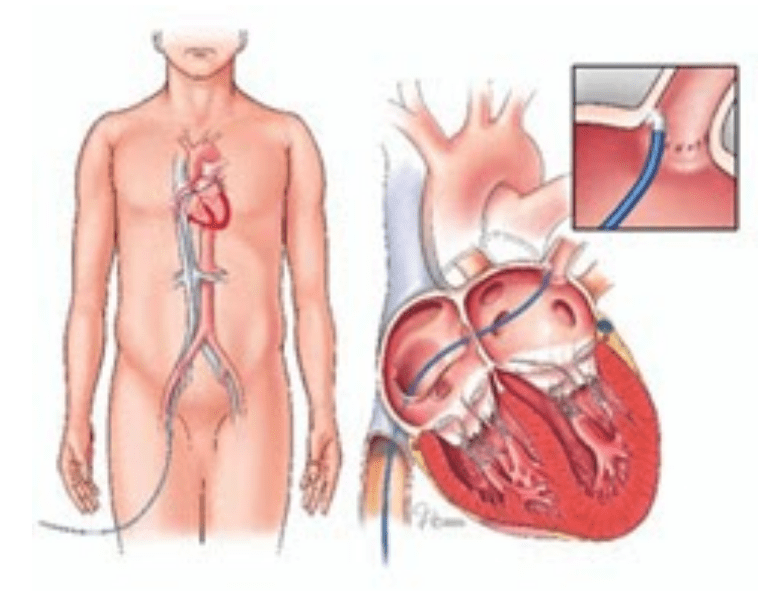
Catheter Ablation for Atrial Fibrillation
Cardiac Surgeons can also treat patients with AF by utilising therapies to ablate the problematic electrical pathways, usually during either open heart or minimally invasive cardiac surgery. This procedure is often referred to as a “Cox-Maze” procedure and involves a MAZE like a pattern ablation of the left atrium when the patient requires cardiac surgery. The goals are the same as a catheter-based ablation, which is to isolate the electrical triggers that may cause AF.
Cardiac Surgeons may also use the following treatment modalities to ablate the desired area of the left atrium:
- Radiofrequency energy
- Cryotherapy
Surgical Ablation for Atrial Fibrillation
Left Atrial Appendage Devices
Within your left atrium, there is a small “pouch” that may allow small amounts of blood to pool and “clot” when patients experience AF. These small clots can leave the heart and flow to other parts of the body and may cause stroke or death in some cases.
In some patients who are unable to tolerate oral anticoagulants (blood thinners), these devices can help reduce the risk of these small clots leaving the heart and causing strokes. These devices are known as Left Atrial Appendage Occlusive devices (LAA) and can be used for specific patient groups who are contraindicated for anticoagulation.
Examples of a left atrial appendage device:
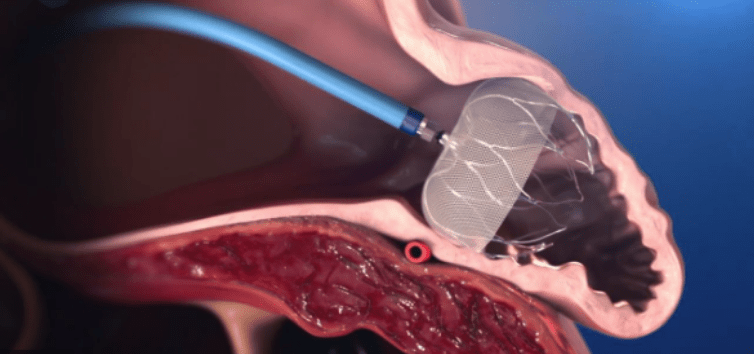
Left Atrial Appendage Closure Device Animation
Ongoing Cardiac Monitoring for Asymptomatic Atrial Fibrillation
Many patients may have AF and not have the typical signs or symptoms such as:
- Shortness of breath,
- Palpitations or racing or fluttering feeling in the chest,
- Decreased exercise tolerance,
- Fatigue,
- Lightheadedness,
- Chest pain10.
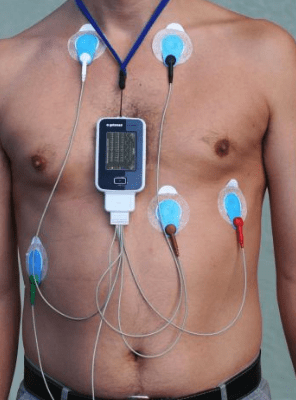
This can lead to many patients being unaware of their risk for stroke and other associated risks of AF. If a doctor suspects that a patient may have AF, then they may require external cardiac monitoring at home to detect if they do have AF. These forms of monitoring may include:
- 24 hour Holter monitoring,
- 7 day Holter monitoring,
- > 7 days Holter monitoring.
These wearable cardiac monitors can record heart rates over the specified period of time and then will be reviewed by a medical team to diagnose if the patient is having periods of AF.
Example of Holter Monitoring
There are also wearable technology monitors that can be worn for short periods of time. This technology can be less restrictive and record your individual heart rate which can be shared via telemetry and other forms of communication with a doctor. These can be used for a number of days and can automatically transmit the relevant information to the patients’ medical team.
Below are some examples of wearable cardiac technology. There are also many smartwatches that have a similar capacity to monitor/ record heart rates that are available. Some of this technology may not be approved in Australia for medical use yet.
Wearable Biosensor Wireless Remote Sensing Device

QardioCore Wearable ECG Monitor