About Mitral Valve Regurgitation
Mitral Valve Regurgitation (MVR) occurs when blood flows backwards into the left atrium through the damaged valve after the left ventricle contracts. This may allow blood to flow in both directions during the ventricular contraction, which can lead to increased pressure within the left atrium, the pulmonary veins, and if severe enough may lead to a build-up of fluid within the lungs. This may deteriorate into signs of heart failure if left undiagnosed and untreated.1
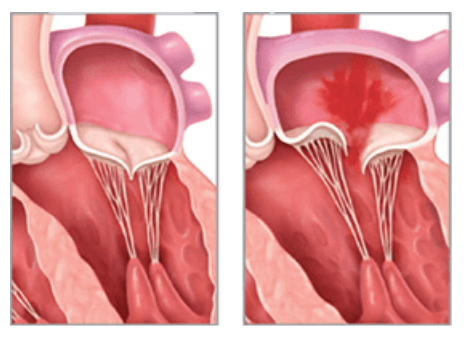
What is Mitral Valve Regurgitation?
Interventional Cardiologist, Dr Ryan Markham explains what mitral valve regurgitation is, what the main causes are and how prevalent this disorder is in the Australian community.
Risk Factors for Mitral Valve Regurgitation
As with many degenerative conditions, age is a common risk factor, however, the following are also risk factors:
- Hypertension,
- Coronary Artery Disease,
- IV drug use,
- Hypertrophic Cardiomyopathy, and
- Congenital heart defects3
Causes of Mitral Valve Regurgitation (MVR)
Mitral valve regurgitation may be caused by a number of different things that can damage and/or reduce the effectiveness of the mitral valve. The condition may be further classified into causes being:
Primary MVR is referring to a physical abnormality with the valve itself:
- Rheumatic fever,
- Chord rupture (tendons around the mitral valve),
- Congenital heart defects,
- Endocarditis,
- Mitral valve prolapse,
- Mitral stenosis.
Secondary MVR refers to conditions that may have damaged the mitral valve such as:
- Trauma,
- Heart attack,
- Heart failure causing cardiomyopathy,
- Hypertension,
- Hypertrophic Cardiomyopathy4
Signs and Symptoms of Mitral Valve Regurgitation
Many people may not present with any signs of mitral valve disease, however, when the disease is advanced symptoms might include:
- Shortness of breath,
- Fatigue,
- Heart murmur,
- Swollen ankles,
- Palpitations,
- Cough,
- Syncope or lightheadedness.
If the atrium is enlarged enough, there may be a predisposition for the patient to experience irregular heart rhythms or atrial fibrillation. This can often be an early diagnostic indication of advanced mitral valve disease.5
Diagnosis of Mitral Valve Regurgitation
Many patients are unaware that they have Mitral Valve Regurgitation and therefore diagnosis might be made incidentally at a routine GP follow up. The first sign may be the presence of a heart murmur, along with the signs and symptoms outlined above.
An Echocardiogram (echo) is the most common testing modality ordered from a GP with a high index of suspicion that heart disease is present. If the presence of the MVR is confirmed, it will typically be classified by its severity, which includes the following:
- Trivial MVR: essentially a normal finding
- Moderate: approximately 30% of blood is flowing backwards during ventricular contraction
- Severe: approximately 50% of blood is flowing backwards during ventricular contraction
- Torrential: the majority of blood is flowing backwards which usually occurs in a ruptured mitral valve.
Additionally, other diagnostic modalities may be used to determine the presence and severity of Mitral Valve Regurgitation. For example, a chest x-ray may be used to identify if an enlarged heart is present. Transoesophageal echo (TOE) and Magnetic Resonance Imaging (MRI) may also be used to indicate the severity of MVR. An Electrocardiograph (ECG) may be performed to identify an irregular heart rhythm (also known as Atrial Fibrillation) but may not have any diagnostic value related to the severity of Mitral Valve Regurgitation.6
What are the symptoms of Mitral Valve Regurgitation?
In the below video, Dr Ryan Markham explains the signs and symptoms of mild to severe mitral valve regurgitation and discusses when patients should be referred on to a Cardiologist for further investigation and possible treatment.
Treatment of Mitral Valve Regurgitation
Dr Ryan Markham from St Andrew’s War Memorial Hospital, explains the process that is taken to treat mitral valve regurgitation in the below video. Including, rating the patient’s dyspnea, reviewing an echocardiogram, and other assessments on the heart.
Medical treatment
Treatment for mitral valve regurgitation will depend on the severity of symptoms and impact on the quality of life, taking into consideration other medical conditions as well. This may be a complex process and involve General Practitioners, Cardiologists, Heart Failure Specialists and other medical professionals to determine what is the most suitable treatment regime for any individual patient.
Patients may be prescribed medications to help alleviate the symptoms of MVR, namely signs of heart failure, and these medications may include:
- Anticoagulants: if irregular heart rhythm (AF) is detected, to prevent the formation of blood clots.
- Diuretics: which may help reduce the fluid accumulation that can occur in patients who have heart failure symptoms associated with MVR
- Blood pressure medications: which may be prescribed to help with reducing high blood pressure that can worsen the effects of MVR in some patients.7
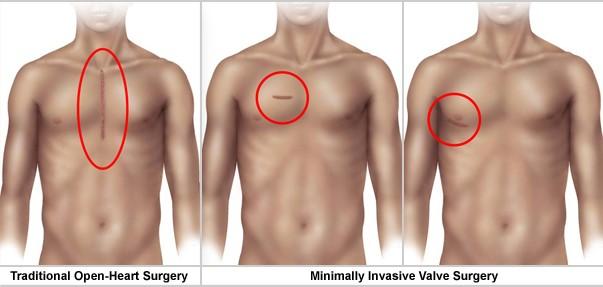
Surgical Treatment of Mitral Valve Repair (MVR)
In some cases, the mitral valve regurgitation is so severe that the mitral valve will need to be replaced or repaired. The decision to repair or replace the damaged valve depends on a number of factors including other pre-existing medical conditions, the age of the patient, as well as, the patients’ ability to rehabilitate after surgery. There are many similarities between aortic valve treatment and mitral valve surgical treatment options.
Types of replacement mitral valves:
There are two main types of surgical mitral valves available:
- Biological tissue valve – which is made from porcine (pig) tissue or bovine (cow) tissue. These biological tissue valves may last 10-15 years on average.
- Mechanical valve – which is made from a carbon-like metal disc that can most likely outlast most patients that receive them. This type of valve may require lifelong anticoagulation to help reduce the risk of blood clot formation.
Surgery may include open-heart surgery or use minimally invasive techniques to replace or repair the damaged mitral valve. Specialist centres can also use a minimally invasive surgical approach with robot-assisted surgery.
Mitral Valve Repair using Catheter Based Therapy
In some cases, patients may not be suitable for an open heart procedure to replace the mitral valve and instead will be more suitable to a less invasive treatment option. This new technique involves a specific tool that aims to reduce the amount of backflow (or regurgitation) in severe mitral valve regurgitation.
It’s performed when a small catheter is inserted within the femoral artery and crosses the septal wall between the right and left atrium, allowing a prosthetic to be deployed in the failing mitral valve. The aim of this device is to bring the mitral valve leaflets closer together to ultimately reduce the amount of regurgitation, backflow that may occur, and symptoms.9
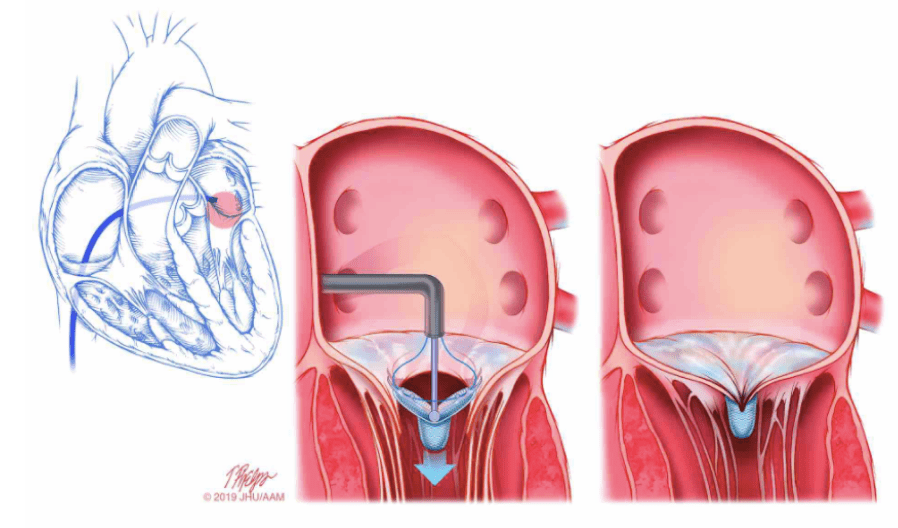
The MitraClip Procedure
The mortality rates and impact on the healthcare system
Lastly, Dr Ryan Markham discusses the impact of undiagnosed and untreated mitral valve regurgitation has on patients and the healthcare system. “Left untreated severe mitral valve regurgitation has a mortality of 57% over a 12 month period… the burden on the healthcare system also follows on from this,” Dr Markham explains in the video below.
