About Coronary Artery Disease
Coronary artery disease refers to diseased coronary arteries that are obstructed or have reduced blood flow due to atherosclerotic plaque which results in decreased blood flow to the heart.
Subsequent reduced blood flow may result in damage to the heart muscle, or referred to as myocardium, commonly referred to as a “heart attack”. This damage is usually irreversible and can affect the normal pumping capacity of the heart, resulting in decreased cardiac output.
What are the signs and symptoms of Coronary Artery Disease?
The most common sign of coronary artery disease is “chest pain” that can occur either at rest or when exercising / moving. Chest pain that occurs whilst exercising, but is relieved when exercise stops may be referred to as “angina.” This is usually a temporary feeling that is caused when the oxygen requirement of the heart is exceeded by the supply which is often due to the presence of coronary artery disease.
Chest pain may also be caused by a reduction in blood flow due to the presence of atherosclerosis or plaque build-up. Cessation of activity or exercise reduces the oxygen requirement of the heart and the myocardial muscle requirement for oxygen, ultimately relieving the pain when resting, typically occurring within a few minutes.
If chest pain is not relieved by rest it may be a sign of ongoing damage to the heart caused by a decreased flow of blood rich oxygen to the heart muscle. This could also be a myocardial infarction or “heart attack.” This may result in a reduction in cardiac output or pumping function and can have long term implications to the patient such as heart failure.
Other signs of coronary artery disease include shortness of breath, palpitations or heart irregularity, sweating, and pain in the patients throat, arms, shoulder, jaw or back.1
What is Coronary Heart Disease?
Diagnosis of Coronary Artery Disease
Patients may often present after to their local Doctor or an Emergency Department after they have experienced a period of chest pain.
The diagnosis of coronary artery disease may be relatively simple or complicated depending on the individual presentation. Diagnostic tests can include:
- 12 lead Electrocardiograph (ECG) which can show signs of electrical changes that are associated with damage to the heart and may indicate which coronary artery may have a potential obstruction due to atherosclerosis or blood clot.
- Blood tests. Heart muscle damage may release specific biomarkers that can be detected in blood tests. Other important measurements from a blood test are cholesterol levels and other electrolytes such as sodium and potassium.
- Exercise Stress Tests is when patients are connected to heart monitors similar to an ECG and their electrical impulses are recorded whilst the patient is exercising, typically whilst on a treadmill. There may be electrical changes indicating a suspicion of coronary artery disease.
- Computerised Tomography Scans (CT scans) can be used to assess the coronary arteries that supply the heart with blood and identify the presence or absence of obstructions, such as plaque, that may limit blood flow to the heart.
- Coronary Angiogram is a procedure where small catheters are inserted into arteries that lead to the heart. These catheters allow Cardiologists to assess the flow and dimensions of the artery and identify obstructions in these arteries. In these procedures, once a lesion (obstruction) is identified, the Cardiologist may insert a stent or other interventional tools to try and maintain or establish normal blood flow through the affected artery. Occasionally there may be multiple arteries that are affected by atherosclerosis and these lesions may require Cardiac Surgery to restore adequate arterial blood flow to the heart.2
What is the treatment of Coronary Artery Disease?
It is important for patients with chest pain or concerns regarding their health to see their General Practitioner or an Emergency Department as soon as possible for assessment. Early intervention can improve patient outcomes.
Treatment for coronary artery disease may depend upon the level of the coronary artery disease the patient has and the urgency of the treatment. This may be defined as managing “Stable” or “Unstable” coronary artery disease.
Treatment for coronary artery disease can vary for each individual and depend on the individual level of risk for coronary artery disease, the presence of coronary artery disease, frequency of symptoms and severity of the disease. A simple method used to treat coronary artery disease may be to reduce the risk of developing coronary artery disease by:
- Implementating simple exercise regimes,
- Dietary changes such as reducing high-fat food intake and increasing the consumption of fruit and vegetables,
- Stopping smoking, or
- Weight reduction / maintenance of a healthy weight range.
Medical management
Medications may be used to assist in the ongoing management of:
- Cholesterol levels,
- Managing Blood pressure if elevated,
- Manage heart failure if present,
- Antithrombotic treatment which aims to stop clots from forming in arteries that have atherosclerotic plaque or an obstruction3
Interventional Management
An Interventional Cardiologist may perform a Coronary Angiogram which is when the coronary arteries are assessed for the presence of obstruction, usually atherosclerotic plaque. Once identified the Cardiologist may decide to insert a type of coronary stent that will maintain adequate flow through the affected coronary artery. There are two main types of coronary stents available currently:
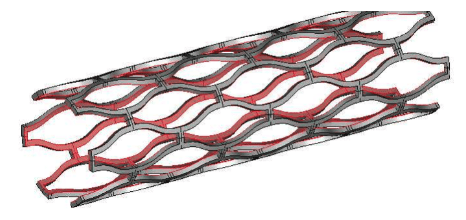
- Bare Metal Stent (BMS) which is a small tube-like structure that’s made of metal and maintains blood flow through the coronary arteries.
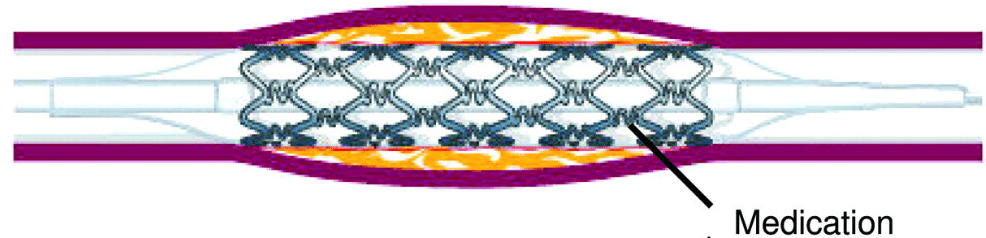
- Drug-Eluting Stents (DES) are similar in structure to bare metal stents but they may have a drug within the frame that slowly infuses out of the stent to reduce complications of thrombus formation and facilitate blood flow through the stent.4
Bare Metal Stent
Drug-Eluting Stent
Cardiac Surgery Procedure for Coronary Arterial Disease
In some cases, the obstruction can be so severe in the coronary artery that open-heart surgery may be considered the most suitable treatment option. In this case, there may be multiple coronary arteries affected by atherosclerotic plaque, causing reduced blood flow to the heart, leading to symptoms. However, the use of multiple coronary stents may not be suitable for all patients.
This procedure is referred to as a Coronary Artery Bypass Graft (CABG) and is performed by a Cardiac Surgeon. Cardiac Surgeons may use blood vessels from various parts of the body to connect these vessels above and below the obstruction, and reinstating a more acceptable arterial blood flow to the heart.
